Afua Twumasi (Cohort 4) is the District Director of Health Services in Ghana, bringing 24 years of experience in the health sector. With 11 years dedicated to clinical care and 13 years to public health, she has a comprehensive understanding of both fields. Afua has served as a district director for 12 years, working across six different districts, demonstrating her leadership and commitment to improving health services in her community.
Q: Can you please give us a brief overview of the current project you’re working on and what you wanted to achieve?
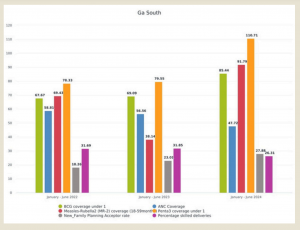
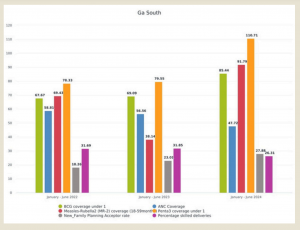
A: My district, the Ga South Municipality, is the second largest district in the Greater Accra region of Ghana. It is also the second largest populated district with low health indicators. My project was to improve health indicators, especially maternal child health indicators within a year, by 20%. The interventions started in 2023. The indicators that have still not improved are Antenatal Care Coverage and Percentage skilled delivery. The emphasis was to improve immunization coverage since there were low immunization rates.
Q: What was the problem?
A: In addressing our organization’s challenges, we identified a critical issue in human resource management: the team was fragmented, and roles were unclear, hindering the effectiveness of our management and health service delivery. To tackle this, we conducted a comprehensive evaluation of the geographic distribution and functionality of our resources, aiming to enhance both management and service delivery. Our solution involved strategic steps such as a thorough Resource Positioning and Assessment to identify critical gaps, followed by Staff Reshuffling based on experience, skills, and knowledge, and implementing targeted Training and Capacity Building to foster a resilient workforce. Collaboration and community engagement were pivotal to our approach. We formed partnerships with private facilities to extend our reach, implemented domiciliary care for children who missed vaccinations, and used Geographic Information Systems (GIS) to analyze health facility distribution and address accessibility issues. By fostering a collaborative work environment and considering risk factors, we ensured regular mop-up operations for vaccinations. This comprehensive approach led to significant improvements in health outcomes and accessibility, creating a cohesive team capable of overcoming challenges and increasing healthcare coverage and efficiency.
Q: What impact do you hope that the Health System Strengthening Project will create?
A: The program aims to create a transformative impact by fostering leadership and improving health service delivery. Through our efforts, I hope to see a team that excels independently, no longer requiring constant oversight. The enhancement of leadership skills has instilled confidence in the team, enabling them to deliver effectively. The work climate has evolved into a collaborative and supportive environment where every team member feels valued. Field supervision has shifted to a more supportive and coaching based approach, resulting in increased motivation and productivity. Witnessing individuals who previously displayed a laissez-faire attitude now actively engage and produce tangible results is particularly rewarding.
Q: What types of skills and knowledge did you find to be the most useful in addressing the situation?
A: Adaptive leadership was crucial in overcoming resistance to change in the public sector, fostering a culture open to change and flexibility. This approach allowed us to manage resistance and stay adaptable to emerging challenges. Our strategy also emphasized monitoring and evaluation, focusing on assumptions and risks to proactively solve problems and implement solutions effectively. Together, adaptive leadership and rigorous monitoring and evaluation significantly enhanced our program’s effectiveness and adaptability, improving outcomes and creating a resilient, dynamic work environment.
Q: What are some of the organizations or stakeholders that you worked with and how did you balance all of them?
A: Different organizations interest In this area, the main stakeholders were staff, mothers, caregivers, community leaders, and religious bodies, whose engagement was crucial due to their influence on women’s participation in health programs. Our team spent five months building local staff capacity to engage stakeholders effectively, organizing community health management committee meetings with leaders to gain support for initiatives like setting up outreach points in community spaces. Engagement was tailored to each community’s context, with sub municipal heads focusing on grassroots engagement and higher-level officials handling broader coordination. We used GIS to identify areas with low immunization coverage, especially in new, rural, and peri-urban settlements, expanding from four to seven sub municipals and improving road accessibility to deliver vaccines. Our program aimed to enhance leadership skills, foster community engagement, and reduce health disparities by ensuring equitable access to health services.
Q: What steps are necessary to implement human resource strengthening programs on a national scale, like the one described?
A: To implement a national human resource strengthening program, government commitment is crucial, along with scientific validation to provide evidence-based results for policy changes. Efficient use of resources is essential, emphasizing effective leadership and team management. Capacity building through on-site training and mentorship ensures practical learning, while pilot programs in selected areas help identify best practices. Disseminating pilot results builds confidence and support and focusing on leadership training fosters strong leaders. Aligning the program with existing policies ensures credibility and effectiveness, leading to improved healthcare outcomes and a more resilient health system.
Q: Anything else that you want to highlight?
A: In my experience working in six districts, including serving as a sub-municipal head, I’ve learned that solving public health problems hinges more on effective leadership than on significant funding. Strong leadership skills, crucial at all levels, can transform limited resources into impressive results, while poor leadership can squander even substantial funds. Building cohesive, motivated teams has been key to success, as dedicated leaders empower their teams to excel by fostering belief in their potential. Though not scientifically tested, my practical experiences consistently show that leadership and team dynamics are core issues in public health, leading to lasting positive outcomes.